The humble Pap Smear is over ninety years old so just to jog your memory, the Papanicolaou test (abbreviated as Pap test, known earlier as Pap smear, cervical smear, or smear test) is a method of cervical screening used to detect potentially pre-cancerous and cancerous processes in the cervix (opening of the uterus or womb).
However, as of December 1st 2017, things are changing with Cervical Cancer Screening in Australia.
Thanks to Dr Kim Pham as originally published by YWCA Victoria!
December brings about a change in Australia’s approach to screening for cervical cancer. Here’s what you need to know about an exciting revolution in health for people with cervixes!!
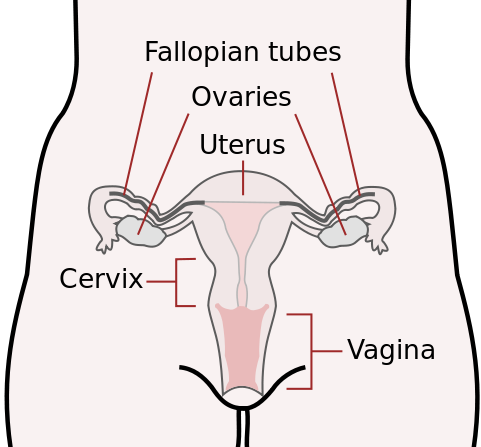
Pap smears involve sampling cells from a specific part of the female anatomy: your cervix. This is the gateway between the vagina and the uterus, and its function is to hold a baby inside your uterus for 9 months: then stretch to let it out!
In order to sample cervical cells, the medical practitioner uses a speculum to view your cervix; but many people consider this examination physically invasive and unpleasant. A pathologist then examines these cells under a microscope for signs of pre-cancerous and cancerous change – what we refer to as cervical cancer. Identifying these changes means you can treat early, preventing more serious disease.
Australia introduced the National Cervical Screening Program in 1991. Since then most cervix-bearing people are prompted by their GP to undergo a pap smear every two years after becoming sexually active. Since its introduction, this program has halved the incidence of cervical cancer in the general population.
The thing is: science is rapidly progressing. Our knowledge of cervical cancer has grown substantially, which has prompted a review of how we screen for abnormal changes. We now know:
-
You need to have contracted a high-risk Human Papilloma Virus (HPV) to get Cervical Cancer.
-
HPV is a viral sexually transmitted infection, like the flu, but downstairs.
-
Infection with HPV is really common! Most people are infected during their lifetime but clear it (like the flu!), with 12% of cervix-owners infected at any given time.
-
Most cervixes infected with high-risk HPV will not develop cervical cancer. The chance of a HPV infection developing into cancer is low.
-
There are 40 recognised types of HPV, but only 15 are currently considered high-risk.
-
Luckily, most HPV infections will cause no symptoms and often are cleared by your immune system.
-
Cervical Cancer develops very slowly and over a number of years.
If you have recently left school, you would recall receiving the HPV vaccination, also known as Gardasil or Cervarix. The National HPV Vaccination Program was introduced in 2007 giving three doses of a vaccination that can protect against two high-risk HPV strains, namely 16 and 18. 71.2% of women in Australia have been vaccinated by the age of 15. Of course, this only works if you haven’t already been exposed to HPV.
Given all this new knowledge, pap smears actually aren’t the most accurate way to measure abnormalities in your cervix! A single test will accurately detect abnormalities in only 40-60% of samples, as it depends on which cells are picked up. This can be improved on with repeated testing (for example, every two years!), but HPV DNA testing is more accurate.
HPV DNA testing involves taking a swab of your cervix, and using genetic assays to look for known DNA that is HPV. It specifically tests for high-risk HPV infections, looking for evidence of the virus from their DNA. This test is better at detecting HPV infection which is the cause of cervical cancer. Using this we can have high confidence that you will not have a HPV infection causing cervical cancer.
Thus, the National Cervical Screening Program is changing to high-risk HPV DNA testing as an alternative to pap smears from the December 2017. This change benefits us because:
-
High-risk HPV DNA testing is more accurate.
-
Less of the people screened will have to undergo further diagnostic or treatment procedures. These are often invasive and potentially damaging to the cervix.
-
You won’t need to be screened as often! Only every five years, and only from 25 years old, until 70 to 74 years old. Of course, if your test is positive you will be required to undergo further investigation, and potentially more regular testing.
-
There is the potential for people to self-collect the specimen, allow those who are uncomfortable with formal collection by a doctor to still participate in the screening program.
That all sounds good, hey? However you may have some other concerns. I’ve tried to address them in the questions below…
If the pap smear is gone, does that mean the procedure is much nicer and less intimate?
No, unfortunately the procedure is almost identical from your perspective, and you will likely notice no difference. All that has changed is its frequency: every five years instead of two. This is one way of reducing how often you have to have a test! The only change to the procedure is exactly how the doctor or nurse collects a sample and its examination by the pathologists.
Wait, if I’m not getting screened before 25 could I have cervical cancer that no one knows about?
As I mentioned, cervical cancer is incredibly rare before the age of 25 and takes a long time to develop. Most women with cervical cancer experience symptoms.
The main symptom is vaginal bleeding in between periods, and/or during or after sex.
Other symptoms include unusual vaginal discharge, discomfort or pain during sex and lower back pain.
If you or someone you know is experiencing these symptoms you should make an appointment with your GP for investigation. Just because we don’t screen everyone below the age of 25, does not mean we will not test you if you have symptoms.
Why do I know women under the age of 25 who have had cancerous or pre-cancerous cells requiring further treatment?
By screening from the age of 25 a number of women will no longer undergo procedures that are unneeded because some abnormal pap smear results may return to normal over time. In fact, 90% of people with HPV clear the infection in two years, and the abnormalities return to normal! Also, evidence shows that screening below the age of 25 don’t reduce the cancer outcomes, as it is so slow to develop.
If they do have persistent infection linked with abnormal changes, they will be detected when screened at the age of 25, which is soon enough – as cervical cancer is incredibly slow in developing. Screening less often will also reduce stress, time, cost and discomfort and risk of complications from treatment of harmless abnormalities.
In addition, given the success of the HPV Vaccination Program, it is anticipated that infection with two major high-risk groups of HPV will decrease, therefore reducing the number of women who would have had abnormal cells in a pap smear.
There a few cases where screening might be considered earlier, in the case of immunocompromised patients or instances of genital contact childhood sexual abuse, which need to be managed on an individual basis.
How do I know if I was vaccinated for HPV?
All teenagers are currently vaccinated from the age of 13. Males began to be vaccinated in 2013, so if you’re past year seven you will not have been vaccinated. For females, if you finished or left school in 2006 you will not have received a HPV vaccination, but beyond that, unless you or your parents declined you’ll have received it. There was a catch up program run, but it ceased a few years ago. If you have not been vaccinated you can pay to have this done as an adult at your local GP.
You can also contact the National HPV Vaccination Program Register if you are unsure. But remember, being vaccinated only prevents against the most common high-risk strains, not all HPV, so cervical screening is still really important!
I’m in a relationship where there are no male sexual organs involved! Does that mean I won’t get HPV?
No! You are at the same risk of HPV in a relationship where sexual contact involves two people with cervixes, as one with a male sexual organ and one with a female. Don’t neglect getting screened!
Isn’t the government just trying to save money reducing how often we are screened?
There are definitely financial benefits for our government in reducing the frequency of screening tests. However, that’s not the main reason for this change. Cervical screening for HPV DNA will be put in place because evidence shows that your cancer will be detected at five-year intervals, and reduce the cost to you in time, money and discomfort of undergoing the examination.
Do you have some published scientific data to back up what you’ve said?
Of course I do! If you’re interested in the government’s process that researched and recommended these changes, head to this website. The documents on this page cite numerous resources made in reviewing our screening program, as well as published research from across the globe. This was developed by the Medical Services Advisory Committee, which is an independent non-statutory committee under the Department of Health. You can learn more about it here.
If you would like further access to specific evidence, please feel free to get in touch!
Further resources:
National Cervical Screening Program
Victorian Cervical Cytology Registry

Your GP at PartridgeGP:
Jo’s Trust – a UK Cervical Cancer Trust that further explores why screening before the age of 25 no longer occurs
Dr Kim Pham is a junior doctor practicing in the northern suburbs of Melbourne. She has an interest in women’s health, sexual health and health advocacy.
Thanks, Kim!
PS: Some extra resources for those seeking extra information

The Screening Pathway
The Cancer Council Video on The Cervical Screening Test with Dr Stella Heley
Government Information for Providers





https://www1.racgp.org.au/newsgp/clinical/self-collection-of-hpv-samples-a-guide-for-gps
Self Collection!
Changes to cervical cancer screening
11 Nov 2021
Australian women eligible for a cervical screening test will be able to collect their own sample from 1 July 2022, offering them more control and choice.
The Australian Government has committed to expanding self-collection of samples to all women under the National Cervical Screening Program from 1 July 2022.
This decision will allow more women to use a simple swab to take a screening sample themselves instead of having a traditional cervical screening test completed by a clinician. Currently, self-collection is only available to women aged 30 years or over, who have never screened, or are two or more years overdue.
For more information, contact the National Cervical Screening team by email: NCSPCommittees@health.gov.au
https://www.health.gov.au/news/self-collection-to-increase-choice-within-the-national-cervical-screening-program